The Pancreas
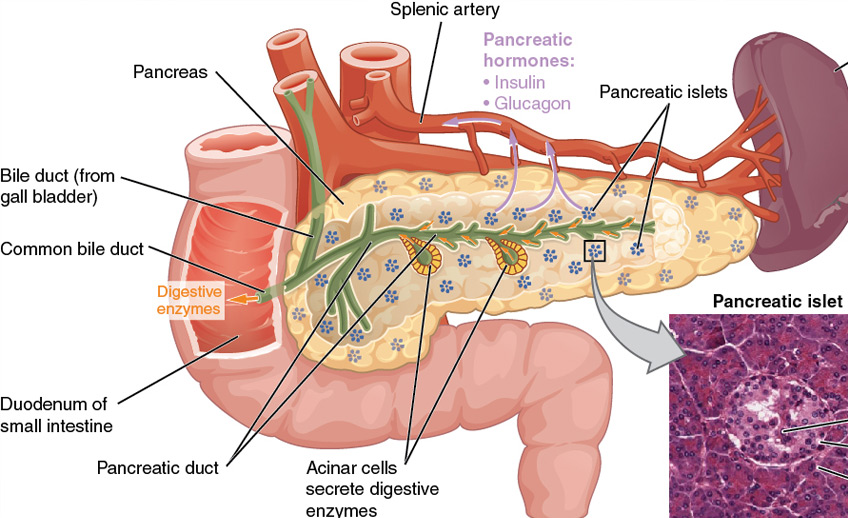
The pancreas is a gland that sits behind your stomach. It plays a key role in
the digestive system. Its juices flow through the pancreatic duct and join bile
from the liver and gallbladder to drain into the small intestine. Specifically,
the pancreas:
- Secretes digestive juice containing enzymes and sodium bicarbonate into the
small intestine. These juices split the fats, proteins and carbohydrates in your
diet into digestible molecules.
- Produces insulin and other hormones that control your body's ability to use sugar (glucose).
- The pancreas is a gland that sits behind the stomach. It plays major roles in
digesting food and controlling your body's use of sugar. Larger than your
gallbladder, but smaller than the liver, the pancreas is an important part of
the digestive system.
- Pancreatitis is inflammation of the pancreas that usually begins as a sudden
attack and is often caused by gallstones or alcohol abuse.
- Symptoms of acute pancreatitis often start with a gradual or sudden severe
pain in the center part of the upper abdomen going through to the back.
- Treatment for pancreatitis often focuses on relieving pain and meeting the
nutritional and metabolic needs of the patient.
- Most people with chronic pancreatitis have a good prognosis if they follow their treatment regimen.
Pancreatitis usually begins as a sudden (acute) attack. When the pancreas becomes acutely inflamed, its digestive enzymes attack the tissue that produces them. One of these enzymes, called trypsin, can cause tissue damage, which causes the pancreas' cells and blood vessels to swell. In some cases, attacks may recur repeatedly, which may cause chronic inflammation and scarring known as chronic pancreatitis.
Exocrine Pancreatic Failure
With chronic pancreatitis, the pancreas may eventually stop producing the enzymes that are necessary for your body to digest and absorb nutrients. This is called exocrine pancreatic failure. Dietary fat and protein may be poorly digested or absorbed, which can result in greasy (oily) stools and weight loss.
Endocrine Pancreatic Failure
When chronic pancreatitis is advanced, the pancreas can also lose its ability to make insulin; this is called endocrine failure and may result in the development of diabetes mellitus.
There are two forms of pancreatitis, but they may not always be distinguishable: acute and chronic.
Acute Pancreatitis
This condition can occur suddenly, soon after the pancreas becomes damaged or irritated by its own enzymes. Although the triggers for acute pancreatitis are not fully understood, its causes are usually gallstones or alcohol abuse. When gallstones pass through the bile duct, they may become stuck and obstruct the pancreatic duct, causing the pancreatic enzymes being produced to build up in the pancreas and ultimately to damage it.
In the case of alcohol, the pancreas may be sensitive to the effects of chronic consumption of excessive alcohol, particularly in smokers. An attack may occur anywhere from a few hours to one to two days after drinking alcohol. The amount of alcohol that needs to be consumed to cause pancreatitis varies from person to person; however, a pattern of excessive daily alcohol use or binge drinking is usually present.
Other less common causes of pancreatitis are:
- High levels of fat particles (triglycerides) in the blood.
- Infections, such as mumps.
- Some medications.
- Certain surgical procedures.
- Heredity (in patients with recurrent attacks of pancreatitis).
- Various other conditions such as diabetes mellitus, celiac disease and elevated blood calcium.
Acute pancreatitis is the leading cause of hospitalization among digestive system
diseases in America. It is responsible for about 270,000 hospitalizations every year.
Chronic Pancreatitis
This form of pancreatitis occurs in patients with a permanently injured or scarred pancreas. Chronic pancreatitis is typically a slowly progressive disease that takes many years to develop. It is often associated with a combination of pain, abnormal digestive function and/or diabetes mellitus.
Chronic pancreatitis is usually due to years of excessive alcohol consumption, but may also result from other causes. Smoking increases the risk of getting chronic pancreatitis.
Differences Between Acute and Chronic Pancreatitis
Most cases of acute pancreatitis are mild and involve a short hospital stay to help heal the pancreas. Chronic pancreatitis is a much more persistent condition. It occurs more often in men than women, particularly when the cause is due to alcohol. Both acute and chronic pancreatitis can be mild or severe and may have the same symptoms.
Often, the only way to distinguish between acute and chronic pancreatitis is to look for visible scar tissue in the pancreas as seen by an abdominal X-ray or other imaging procedures. Your physician will also look for evidence of chronic damage to the pancreas (such as greasy stools because it is not producing digestive enzymes) and unexplained weight loss.
Acute and Chronic Pancreatitis Symptoms
Symptoms include:
- A gradual or sudden severe pain in the center part of the upper abdomen going
through to your back; this pain may get worse when you eat and builds to a
persistent pain.
- Nausea and vomiting.
- Fever.
- Jaundice (a yellowing of the skin) due to blockage of the bile duct from the
inflamed pancreas.
- Skin nodules due to leakage of digestive enzymes into the blood causing soft
tissue injury at sites with fat deposition.
- Weight loss (with chronic pancreatitis).
- Greasy or oily stools (with chronic pancreatitis).
Patients who have recurrent or chronic pancreatitis for many years may be at an increased risk for developing cancer of the pancreas. This is a rare event. Acute pancreatitis has not been shown to increase the risk of pancreatic cancer. However, it can be a manifestation of pancreatic cancer particularly in the elderly without an obvious cause of acute pancreatitis.
If you have unexplained weight loss that lasts more than a few weeks, call your doctor. If You Think You Have Pancreatitis
Call your doctor. Your doctor will:
1. Take a medical history, including the medications you take.
2. Ask about your drinking and cigarette smoking history.
3. Draw blood to test for pancreatic enzyme levels.
4. Order an X-ray or other imaging test to determine the degree of pancreas damage.
Acute Pancreatitis Treatment
Your doctor will usually admit you to the hospital to receive intravenous fluid hydration, treatment of pain and monitoring for complications. Nothing-by-mouth status will be maintained until pain resolves and there is no nausea or vomiting, typically a few days.
Most cases of acute pancreatitis resolve within a week. For persistent symptoms additional treatments may be necessary.
In addition:
- If the cause of acute pancreatitis is gallstones, you will typically be
advised to have your gallbladder removed to prevent further attacks.
- If the bile duct is found to be enlarged, you may need a procedure called ERCP
to drain it. An ERCP is a way your doctor can examine your pancreas, pancreatic
duct, the bile ducts and/or the sphincter of Oddi (the muscle that controls the
flow of pancreatic juices and bile into the intestine). In severe cases, surgery
will be required to drain the pancreatic duct or to remove part of the pancreas.
- Your doctor will give you dietary guidelines to follow in order to reduce the
amount of fats you eat, since your body has trouble digesting these substances.
- You may also need to take pancreatic enzyme supplements with every meal. These
supplements will help your body absorb food, and help you regain some of
the lost weight. The low-fat diet and the enzyme supplements may also help
control pain by reducing stimulation of the pancreas.
- If you drink alcohol, you need to stop drinking.
- If you smoke cigarettes, you need to stop smoking.
- If you have a pancreatic pseudocyst, it may need to be drained.
While pancreatitis is still not fully understood, there are some steps you can take to prevent it from occurring again:
- If the cause is gallstones and your gallbladder has not been removed, avoid
fatty and greasy foods, such as butter and fried eggs.
- Work with your gastroenterologist to develop a healthy eating plan.
- Ultimately, you may need your gallbladder removed. Your doctor should help you
decide whether this surgery is needed.
- If the cause is alcohol, you should stop drinking altogether.
- If you smoke cigarettes, you should stop smoking altogether.