CELIAC DISEASE OVERVIEW
Celiac disease is a condition in which the
immune system responds abnormally to a protein
called gluten, which then leads to damage to the
lining of the small intestine. Gluten is found
in wheat, rye, barley, and a multitude of
prepared foods. Celiac disease is also known as
gluten-sensitive enteropathy and celiac sprue.
The small intestine is responsible for absorbing
food and nutrients. Thus, damage to the lining
of the small intestines can lead to difficulty
absorbing important nutrients; this problem is
referred to as malabsorption. Although celiac
disease cannot be cured, avoiding gluten usually
stops the damage to the intestinal lining and
the malabsorption that results. Celiac disease
can occur in people of any age and it affects
both genders.
CELIAC DISEASE
SYMPTOMS
The symptoms of celiac
disease vary from one person to another. In its
mildest form, there may be no symptoms
whatsoever. However, even if you have no
symptoms, you may not be absorbing nutrients
adequately, which can be detected with blood
tests. As an example, you can develop a low
blood count as a result of decreased iron
absorption.
Some people have bothersome
symptoms of celiac disease, including diarrhea,
weight loss, abdominal discomfort, excessive
gas, and other signs and symptoms caused by
vitamin and nutrient deficiencies.
Some
conditions are more common in people with celiac
disease, including:
- Osteopenia or
osteoporosis (weakening of the bones)
- Iron
deficiency anemia (low blood count due to lack
of iron)
- Diabetes mellitus (type I or
so-called juvenile onset diabetes mellitus)
-
Thyroid problems (usually hypothyroidism, an
underactive thyroid)
- A skin disease called
dermatitis herpetiformis
- Nervous system
disorders
- Liver disease
CELIAC DISEASE CAUSES
It is not
clear what causes celiac disease. A combination
of environmental and genetic factors is
important. Celiac disease occurs widely in
Europe, North and South Americas, Australia,
North Africa, the Middle East, and in South
Asia.
Celiac disease occurs rarely in
people from other parts of Asia or sub-Saharan
Africa.
CELIAC DISEASE DIAGNOSIS
Celiac disease can be difficult to diagnose
because the signs and symptoms are similar to
other conditions. Fortunately, testing is
available that can easily distinguish untreated
celiac disease from other disorders.
Blood tests - A blood test can
determine the blood level of antibodies
(proteins) that become elevated in people with
celiac disease. Over 95 percent of people with
untreated celiac disease have elevated antibody
levels (called IgA tissue transglutaminase, or
IgA tTG), while these levels are rarely elevated
in those without celiac disease. Levels of other
antibodies (called IgA or IgG deamidated gliadin
peptide) are also usually abnormally high in
untreated celiac disease. Before having these
tests, it is important to continue eating a
normal diet, including foods that contain
gluten. Avoiding or eliminating gluten could
cause the antibody levels to fall to normal,
delaying the diagnosis.
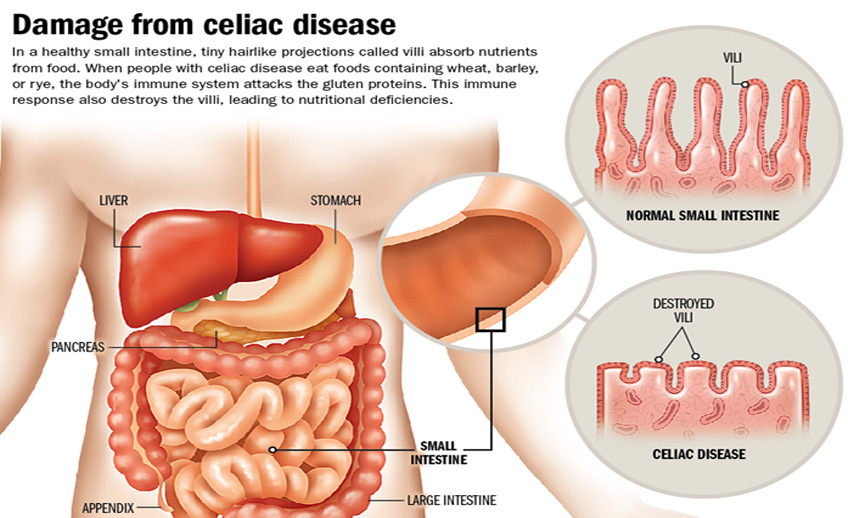
Small
intestine biopsy - If
your blood test is positive, the diagnosis must
be confirmed by examining a small sample of the
intestinal lining with a microscope. The sample
(called a biopsy) is usually collected during an
upper endoscopy, a test that involves swallowing
a small flexible instrument with a camera. The
camera allows a physician to examine the upper
part of the gastrointestinal system and remove a
small piece (biopsy) of the small intestine. The
biopsy is not painful. In people with celiac
disease, the lining of the small intestine has a
characteristic appearance when viewed with a
microscope. Normally, the lining has distinct
finger-like structures, which are called villi.
Villi allow the small intestine to absorb
nutrients. The villi become flattened in people
with celiac disease. Once you stop eating
gluten, the villi can resume a normal growth
pattern. More than 70 percent of people begin to
feel better within two weeks
after stopping
gluten.
One way to determine if
the gluten-free diet is working is to monitor
the levels of antibodies in your blood. If your
levels decline on a gluten-free diet, this
usually indicates that the diet has been
effective.
"Potential" celiac
disease - People with a positive IgA
endomysial antibody test and/or a positive IgA-tTG
test and a normal small bowel biopsy are
considered to have potential celiac disease.
People with potential celiac disease are not
usually advised to eat a gluten-free diet.
However, ongoing monitoring (with a blood test)
is recommended and a repeat biopsy may be needed
if you develop symptoms. Biopsies should be
taken from several areas in the bowel since the
abnormality can be patchy.
"Silent" celiac disease - If you have a
positive blood test for celiac disease and an
abnormal small bowel biopsy, but you have no
other symptoms of celiac disease, you are said
to have "silent" celiac disease. It is not clear
if people with silent celiac disease should eat
a gluten-free diet. Blood tests for
malabsorption are recommended, and a gluten-free
diet may be needed if you have evidence of
malabsorption.
Testing for
malabsorption - You should be tested
for nutritional deficiencies if your blood test
or bowel biopsy indicates celiac disease. Common
tests include measurement of iron, folic acid,
or vitamin B12, and vitamin D. You may have
other tests if you have signs of mineral or fat
deficiency, such as changes in taste or smell,
poor appetite, changes in your nails, hair, or
skin, or diarrhea.
Other tests
- Other standard tests include a CBC (complete
blood count), lipid levels (total cholesterol,
HDL, LDL, and triglycerides), and thyroid
levels. Once your celiac antibody levels return
to normal, you should have a repeat test once
per year.
Many clinicians recommend a test for bone
loss 12 months after beginning a gluten-free
diet. One method involves using a bone density
(DEXA) scan to measures your bone density. The
test is not painful and is similar to having an
x-ray. If you have significant bone loss, you
may need calcium and vitamin D supplements, an
exercise program, and possibly a medicine to
stop bone loss and encourage new bone growth.
CELIAC DISEASE COMPLICATIONS
Nonresponsive celiac disease -
Approximately 10 percent of people with celiac
disease experience ongoing symptoms despite
adhering to a gluten-free diet. There are many
causes, including other food intolerances such
as fructose (or other fermentable carbohydrate)
malabsorption, food allergies, bacterial
overgrowth in the small intestine or conditions
such as microscopic colitis, irritable bowel
syndrome, pancreatic exocrine insufficiency, or
refractory celiac disease. However, the most
common cause is ongoing, often inadvertent,
gluten ingestion. Thus, an essential first step
in evaluating nonresponsive celiac disease is
consultation with an experienced celiac
dietitian.
Refractory celiac
disease - A small percentage of people
develop intestinal symptoms that do not improve
despite use of a strict gluten-free diet. In
other cases, intestinal symptoms initially
improve with dietary changes but then return.
People who have these problems may have
refractory celiac disease. The cause of this
problem is not known. Treatment involves
medications that suppress the immune system's
abnormal response (eg,
steroids). Treatment is important
because
people with untreated celiac disease can develop
anemia, bone loss, and other consequences of
malabsorption.
Ulcerative
jejunitis - People with refractory
celiac disease who do not improve with steroids
(glucocorticoids) may have a condition known as
ulcerative jejunitis. This condition causes the
small intestine to develop multiple ulcers that
do not
heal; other symptoms may include a
lack of appetite, weight loss, abdominal pain,
diarrhea, and fever. This condition can be
difficult to treat. Treatment may require
surgery to remove the ulcerated area.
Lymphoma - Cancer of the
intestinal lymph system (lymphoma) is an
uncommon complication of celiac disease.
Avoiding gluten can usually prevent this
complication.
Skin conditions - Celiac
disease is associated with a number of skin
disorders, of which dermatitis herpetiformis is
the most common. Dermatitis herpetiformis is
characterized by intensely itchy, raised,
fluid-filled areas on the skin, usually located
on the elbows, knees, buttocks, lower back,
face, neck, trunk, and occasionally within the
mouth.
The most bothersome symptoms are
itching and burning. This feeling is quickly
relieved when the blister ruptures. Scratching
causes the area to rupture, dry up, and leave an
area of darkened skin and scarring. The
condition will improve after eliminating gluten
from the diet, although it may take several
weeks to see significant improvement. In the
meantime, an oral medication called dapsone may
be recommended. Dapsone relieves the itching but
does not heal the lining of the small intestine;
thus, the gluten-free diet is the most effective
therapy for those with dermatitis herpetiformis.
CELIAC DISEASE TREATMENT
Gluten-free diet - The cornerstone of treatment
for celiac disease is complete elimination of
gluten from the diet for life. Gluten is the
group of proteins found in wheat, rye, and
barley that are toxic to those with celiac
disease. Gluten is not only contained in these
most commonly consumed grains in the Western
world, but is also hidden as an ingredient in a
large number of prepared foods as well as
medications and supplements. Maintaining a
gluten-free diet can be a challenging task that
may require major lifestyle adjustments. Strict
gluten avoidance is recommended since even small
amounts can aggravate the disease. It is
important to avoid both eating gluten and being
exposed to flour particles in the air.
Get help from a dietitian - An
experienced celiac dietitian can help you to
learn how to eat a gluten-free diet, what foods
to avoid, and what foods to add for a
nutritionally balanced diet. Your dietitian can
also recommend gluten-free vitamin/mineral and
other supplements, as needed. Your celiac
dietitian can also educate you on shopping, food
preparation, and lifestyle resources. Excellent
resources are also available from celiac medical
centers, organizations, and support groups.
Fortunately, life on a gluten-free diet becomes
increasingly easier each year due to the rising
popularity of gluten-free foods among those with
celiac disease, nonceliac gluten sensitivity,
and wheat allergies. Excellent gluten-free
substitute foods are now widely available in
supermarkets, health food stores, and online.
General tips
Avoid foods
containing wheat, rye, barley, malt, brewer's
yeast, oats (unless pure, uncontaminated,
labeled gluten-free oats), and yeast extract and
autolyzed yeast extract (unless the source is
identified as gluten-free). "Malt" means "barley
malt" unless another grain source is named, such
as "corn malt." The US Food and Drug
Administration (FDA) and the United States
Department of Agriculture have different
regulations around gluten-free food labeling.
According to the FDA regulations issued in
August 2013, foods with "gluten-free" labeling
must contain less than 20 parts per million
(ppm) of gluten. The following table has a list
of prepared foods that contain or may contain
gluten. Naturally gluten-free foods include
rice, wild rice, corn, potato, and other foods
listed in the table. These foods may be
contaminated with wheat, barley, or rye. Choose
labeled gluten-free versions of these products.
Exceptions are fresh corn, fresh potatoes, nuts
and seeds in their shells, dried lentils
(legumes), and dried beans. These foods may not
be labeled gluten-free but are still considered
safe to eat. Pick through and rinse dried
legumes and dried beans.
If a food is
regulated by the FDA and is not labeled
gluten-free (such as prepared foods and
condiments), read the ingredients list and
"contains" statement carefully. The word "wheat"
will be included if the product is FDA regulated
and contains wheat protein. If you do not see
any of the following words on the label of an
FDA-regulated food (wheat, rye, barley, malt,
brewer's yeast, oats, yeast extract, and
autolyzed yeast extract) then the product is
unlikely to include any gluten-containing
ingredients. However, the Food Allergen Consumer
Protection Act pertains to ingredients only. It
does not cover wheat protein that may be in a
product unintentionally due to cross-contact.
Distilled alcoholic beverages and vinegars, as
well as wine, are gluten-free unless
gluten-containing flavorings are added after
production. However, malt beverages, including
beer, are not considered gluten-free. There are
specially produced beers that do not use malted
barley that are labeled gluten-free and can be
consumed on a gluten-free diet. Please note that
malt vinegar is not gluten-free.
You may
not tolerate dairy products initially while your
intestines are healing. If you tolerated lactose
before your diagnosis, you may be able to
tolerate it again after the intestine heals. In
the meantime, choose lactose-reduced or
lactose-free products if your symptoms are
worsened by dairy products. Choose labeled
gluten-free, dairy-free alternatives, such as
rice, soy, or nut (almond, hazelnut) beverages
that are enriched with calcium and vitamin D.
Keep in mind that gluten-free rice and nut milks
have minimal protein per serving compared with
cow's or soy milk. Gluten-free lactase enzyme
supplements are also available, which may help
you to tolerate foods that contain lactose.
Discuss your need for calcium and vitamin D
supplements with your healthcare provider or
dietitian. A small percentage of people with
celiac disease cannot tolerate gluten-free oats
for several reasons. If you choose to eat
gluten-free oats, first talk to your doctor who
can check your IgA-tTG level and monitor any
symptoms. In addition, choose only specially
produced gluten-free oats. Limit your intake of
gluten-free oats to no more than 50 grams
(approximately 1/2 cup dry rolled oats or 1/4
cup dry steel-cut oats) per day. If tolerated,
you may be able to discuss eating more than 1/2
cup per day under the supervision of your
doctor.
Is gluten avoidance
really necessary? - People who have no
symptoms of celiac disease often find it
difficult to follow a strict gluten-free diet.
Indeed, some healthcare providers have
questioned the need for a gluten-free diet in
this group. However, certain factors support a
gluten-free diet, even in those without
symptoms: Strictly following a gluten-free diet
sometimes helps you to feel more energetic and
have an improved sense of health and wellbeing.
Some people with celiac disease have vitamin or
nutrient deficiencies that do not cause them to
feel ill, such as anemia due to iron deficiency
or bone loss due to vitamin D deficiency.
However, these deficiencies can cause problems
over the long term.
Untreated celiac
disease can increase the risk of developing
certain types of gastrointestinal cancer. This
risk can be reduced by eating a gluten-free
diet.
IMPLICATIONS FOR THE FAMILY
Eliminating gluten requires a major lifestyle
change for you as well as your family. However,
with time and practice, it will be easier to
know which foods, medications, supplements, and
oral care products contain gluten and what
alternatives are available. Although eating out
can be challenging initially, restaurants have
become increasingly interested in serving people
with celiac disease by offering a gluten-free
menu or ingredient substitutions. Families also
need to be aware of their increased risk of
celiac disease. Thus, your first-degree
relatives (parents, brothers, sisters, children)
should consider being tested, especially if
anyone has signs or symptoms of the condition.
Testing is typically done with a blood antibody
test, as described above.